Definition
The adenomatoid odontogenic tumor is a relatively uncommon,well-circumscribed,odontogentc neoplasm charactezed by the formation of multiple ‘ducts-like’ structures by the neoplastic epithelial cells.
The name ‘adenomatoid’ has been given to the neoplasm because histologically numerous duct-like are often intersersed thorough out the lesion give glandular or matoid apprarance to it.
Origin
The tumor probably arises from the reduced enamel epithelium,during the presecretory phase of enamel organ development.Some investigators believe that the neoplasm develops from a pre-existing dentigerous cyst.
Clinical Features
Age-The tumor usually occurs in the younger age (e.g.second and third decade of life) Rarely it can occur in the older age.
Sex-Females are more commonly affected in comparison to the males.
Site-The lesion most typically occurs in the maxillay amterior region (upper laterag incisor-canine area) Rarely it involves the mandeble in the angle -ramus area in about 70% cases the neoplasms occur in association with an unrupted tooth , Some lessions develop extra orally in relation to the gingiva.
Clinical Presemtation
Differential Diagnosis
Histopathological Feature
Treatment
By surgical enucleation . The associated tooth has to be removed and recurrence is rare.
The adenomatoid odontogenic tumor is a relatively uncommon,well-circumscribed,odontogentc neoplasm charactezed by the formation of multiple ‘ducts-like’ structures by the neoplastic epithelial cells.
The name ‘adenomatoid’ has been given to the neoplasm because histologically numerous duct-like are often intersersed thorough out the lesion give glandular or matoid apprarance to it.
Origin
The tumor probably arises from the reduced enamel epithelium,during the presecretory phase of enamel organ development.Some investigators believe that the neoplasm develops from a pre-existing dentigerous cyst.
Clinical Features
Age-The tumor usually occurs in the younger age (e.g.second and third decade of life) Rarely it can occur in the older age.
Sex-Females are more commonly affected in comparison to the males.
Site-The lesion most typically occurs in the maxillay amterior region (upper laterag incisor-canine area) Rarely it involves the mandeble in the angle -ramus area in about 70% cases the neoplasms occur in association with an unrupted tooth , Some lessions develop extra orally in relation to the gingiva.
Clinical Presemtation
 |
| AOT Enucleation Surgery Image via: www.dental.washington.edu |
- The tumor usually presents a slow enlarging , small ,bony hard swelling in the maxillary anterior region.
- Sometime it can occur in the premolar region k.
- The lession often causes elevation of the upper lip on the involved side ,which often resuts in a change in the facial profile.
- Dislacement of the regional teeth , mild pain and expansion of the cortical bone are usually present.
- If the lesion is very large it may cause severe expansion of the which may sometime elicit fluctuation.
- In many cases, the lesion is asymptomatic in nature and it is often associated with an uperupted tooth (mostly the upper canine)
- Occasionally adenomatoid odontogenic tumor may occur extra-ossously in the anterior maxilly gingiva and it prodeces a solirary painless , asymptomatic nodular swelling.
 |
| AOT of mandibular left canine region image via: jaypeejournals.com |
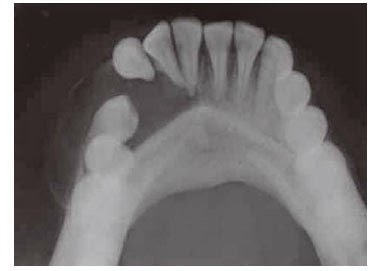
- Radiographically adenomaroid odontogenic tumor presents a well-defined , unilocular,radiolucent area,which is often enclosing a tooth or tooth-like stucture.
- Multiple small,radiopaque foci of varying radiodensity may be predent inside the lesion .
- Expansion of the distrotion of the cortical plates and displacement of the roots of the adjoining teeth are sometime seen.
- The border of the lesion is not well corticated and it consistently engulfs the impacted tooth including its root.This feature differentiates adenomataid adontogenic tumor from dentigerous cyts,since the later lession encloses only the crown portion of on impacted tooth.
Differential Diagnosis
- Dentigerous cyts
- Globulomaxillry cyts
- Lareral periodontal cyts
- Odontome
- Unicystic ameloblastoma
- Ossiffying or cementifying fibroma
- Calcifying epithelial odontogenic tumor
- Calcifyinh epithelial odontogenic cyts.
Histopathological Feature
- Microscopically, adenomatoid odontogenic tumor reveals neoplastic odontogenic epithealial cells,proluferating in multiple "duck-like" patterns,within a thin but well-vascularized stroma.
- The presence of these duck-like strucrures often give the lesion an adenomatoid or glandular apperance.
- Each dick-like structure is bordered on the periphery by a single layer of tall columnar cell resembling ameloblasts.
- Serial sectioning reveals that the lumens are blind ended ang they probably represent an abortive attempt at anamel oraga formation.
- The lumen of the duck-like structures are filled with a homogenous eosinophilic coagulum.
- Small foci of calcification are often seen , which are scattered throughout the lesion.
- In some cases , the neoplastic cells are arranged in solid nests or rosettem and these cells simetime may fill up the entire lumen of few ducts.
- Droplets of amorphous (PAS prositiv) eosino philic materials are frequently found in between the neoplastic calls.
- In some adenomatoid odontogenic tumos tubular dentin or enamel matrix may also be found.
- The neoplasm is almost always well-encap sulated and the connective tissue stroma may occasionally contain diffuse areas of hyaline materials.
Treatment
By surgical enucleation . The associated tooth has to be removed and recurrence is rare.






